Step 1: Determine if you're eligible
Psychologists and licensed clinical social workers are eligible clinician types to receive the MIPS payment adjustment.
MIPS eligibility exemptions
- 1Participation in an Advanced Alternative Payment Model (APM) Eligible clinicians who are part of an Advanced APM are exempt from MIPS reporting. Current examples of APMs are certain Accountable Care Organizations (ACO) and bundled payment models.
- 2MACRA Quality Payment Program Low-Volume Threshold
Eligible clinicians or groups will be exempt from MIPS reporting if they bill ≤ $90,000 or provide care for ≤ 200 Medicare Part B patients or if they have ≤ 200 covered professional services. Clinicians that meet 1 or 2 (but not all 3) of these criteria may opt in to be eligible for MIPS penalties and incentives. - 3Newly enrolled in Medicare
You may be required to report to MIPS if you bill Medicare Part B claims under a new practice/TIN in segment 2 of the MIPS Determination Period or join an APM Entity in later snapshots.
Step 2: Understand reporting
The MIPS payment adjustment
Much like the sunset Value-Based Payment Modifier Program (VM), MIPS determines each eligible clinicians’ payment adjustment based on how they rank versus their peers. The score used to determine the performance threshold for MIPS is called the MIPS Composite Performance Score, or the MIPS final score. This score is calculated on a scale from 0-100 and consists of the aggregated performance from the 4 MIPS performance categories.
Unlike past quality initiatives, a clinician's MIPS payment adjustment will now follow them even after they depart from the TIN they reported under.
Physician Compare
In addition to impacting eligible clinicians financially, MIPS performance has the potential to affect the reputation of eligible clinicians and groups. Scores will be publicly posted to Physician Compare as soon as the informal review period closes following the performance year.
Step 3: Review performance categories
Quality
To successfully report the Quality performance category, participants must report 6 measures (1 of which is an outcome measure) over a full calendar year for at least 75% of the applicable patient visits.
Promoting Interoperability
The Promoting Interoperability performance category is updated to be more flexible, customizable, and focused on patient engagement and interoperability. To receive credit in PI, participants must attest to all base score PI measures. Full credit will only be awarded to participants who also report performance score measures in addition to base score measures.
Improvement Activities
The Improvement Activities performance category rewards eligible clinicians for participating in activities related to their patient population. Clinicians and groups can choose to participate in activities most relevant to both their practice and patient population.
Cost
The Cost performance category is computed at a clinician group level, based on meeting minimum episode thresholds for each measure. All cost measures are automatically captured through administrative claims.
Step 4: Start with MBHR by MIPSpro
Under MIPS, performance matters. It's no longer enough to just report quality data. In 2024, CMS penalties could be as high as minus-9%, while incentives will be available for high performers. Although Medicare quality reporting is complicated, MBHR makes the reporting process easy with an intuitive system and a quality reporting team to guide you through the MIPS reporting process and to success
MBHR delivers key features to ensure your success:
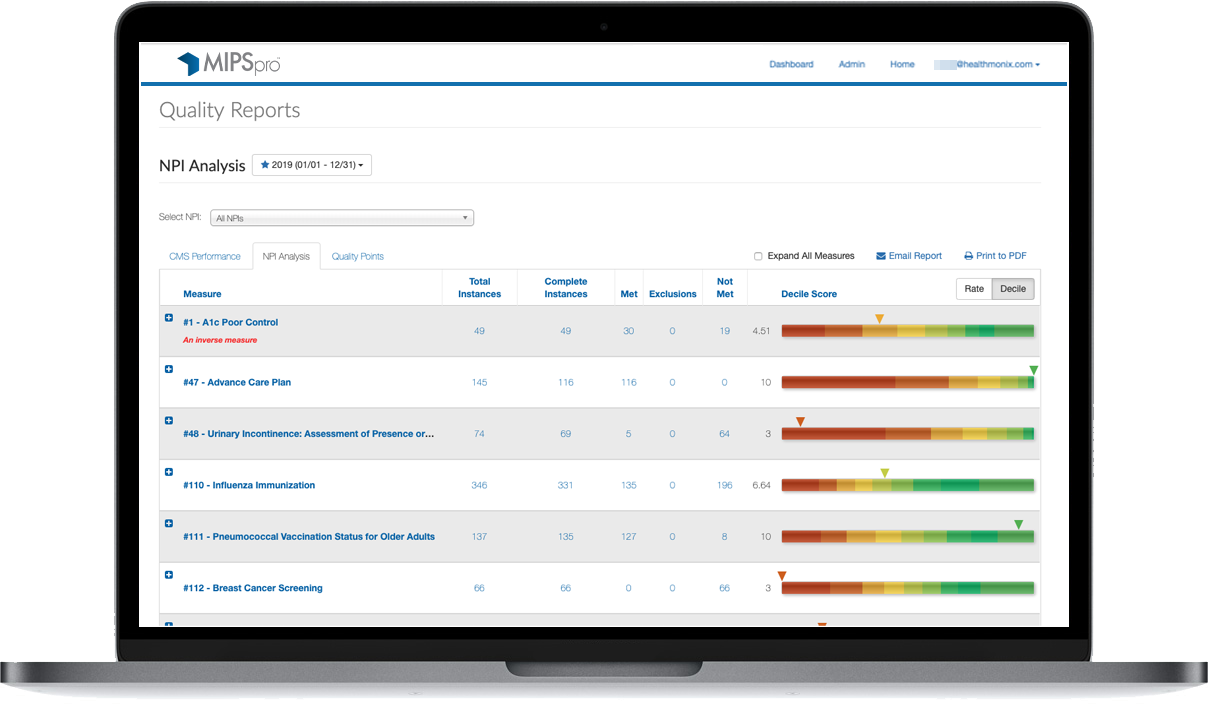
Real-time dashboards
MIPS Quality, PI, IA and Cost performance categories for all specialties and measures
Adaptable to your practice
Ability to choose your reporting pace

Integrated data
Data validation and support
